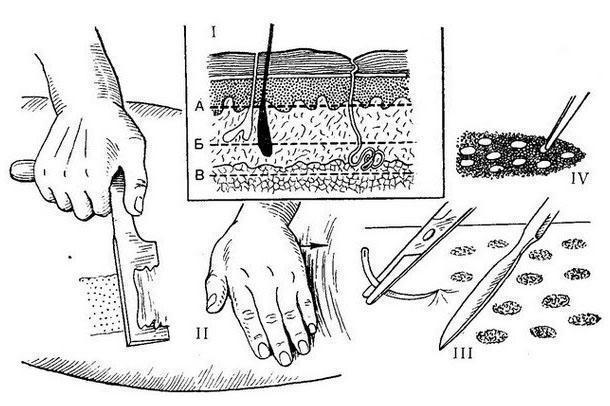
Zh. Reverden (1869) transplanted small areas of the epidermis with an area of 2-6 mm2 onto the granulating surface. S. M. Yanovich-Chainsky (1870) transplanted skin grafts with a size of 4 -12 mm2 containing the epidermis and part of the dermis, for the first time successfully applying this method of CP to close defects after gunshot wounds. J. S. Davis (1914) transplanted skin grafts that included up to 3⁄4 of the entire thickness of the skin. Tiersch (K. Thiersch, 1874) proposed a thin split graft containing only the epidermis. Small thin strips of the epidermis were cut off with a special knife and transplanted into granulating wounds. Ollier (L. Oilier, 1872)produced plastic grafts of large sizes, up to 4-8 cm2, later he used grafts for the entire thickness of the skin for the CP. Blair (V. P. Blair) and Brown (J. V. Brown, 1929) used a manual method of splitting the skin, with the help of which they were able to obtain dermoepithelial grafts of various areas with a thickness of 0.3— 0.4 mm. Dermatomic CP is widely used with a split calibrated graft, i.e., with a pre-planned thickness. In our country, K. The works of H. N. Blokhin, B. A. Petrov, M. V. Kolokoltsev, E. I. Shumilkina, T. Ya. Aryev, A. K. Tychinkina and other surgeons are devoted to the split dermatome graft surgery. In dermatomic CP, thin skin grafts are placed on a previously prepared wound surface and covered with a pressure bandage. On the second day, be sure to make a careful change of the dressing in order to avoid displacement of the graft with a dried bandage. Thicker dermatomic grafts are used for CPR purposes on the face, palmar surfaces of the hands, in the area of the joints and plantar surfaces of the feet. The area of the skin used for plastic surgery (donor) is covered with a sterile bandage; it can be reused for CP after 8-10 days, and if necessary repeatedly, which is especially important in the treatment of extensive burns.
B. A. Petrov (1950), R. Mowlem (1952), and D. Jackson (1952) used tape - shaped alternating split auto-and homotransplants to close wounds after extensive burns. CP was performed at the end of the 3rd week after the burn. Auto-and homotransplants covered the entire wound surface. Homotransplants slowly dissolve, autotransplants, gradually expanding to the sides, cover the granulations. Thin flaps with a thickness of 0.1—0.2 mm are used; they take root better than thick ones, do not require fixing to the edges of the wound and are almost not subject to retraction. With an insufficient supply of skin, with extensive burns, Gabarro (P. Gabarro, 1943) proposed a “vintage” method of CP— small rectangular grafts placed on the wound surface at different intervals.
The full-layer free CP was proposed by Lawson (G. Lawson, 1870) and A. S. Yatsenko (1871). Graft sizes are 2-4-6 mm2. Krause (F. Krause) in 1893 used grafts up to 20— 25 cm2 for CP.
Pyasetsky (1870) for better engraftment, skin grafts were immersed in wells, which were previously made in granulations. This “immersion” method of skin grafting was later improved by Brown (W. Braun, 1920) and Alglave (P. Alglave, 1927). Brown transplanted small epidermal grafts with a needle under the granulation. Alglav immersed full-layer skin grafts under granulations or in wells created by scraping out the granulations. A perforated flap-screen is used to close large skin defects. Douglas first applied circular incisions in the graft area, after which the skin flap was separated, leaving round areas of skin for epithelization of the donor wound. Dragstedt and Wilson performed linear incisions on the skin graft. The donor wound was sewn tightly. The creation of holes in the graft contributed to a good drainage of the wound and allowed to increase the area of the graft.
One of the varieties of full-layer free CP is the replantation of skin flaps on the wound, completely torn off at the time of injury, proposed by V. K. Krasovitov in 1935. The method of replanting skin flaps according to Krasovitov for scalped wounds of the head and limbs is successfully used in emergency surgery. In case of contamination, the scalped skin is washed with soap and a brush in running water, oil stains are removed with ether, after which the skin flap is immersed in rivanol solution.
The subcutaneous tissue is removed with a dermatome, the skin flap is dried and transplanted to the wound. Skin replantation is allowed within 6 hours after the wound, but methods have been developed to significantly extend the time for maintaining the viability of the separated skin flap.
Be the first to post a message!