Also known as “concussion,” chronic traumatic encephalopathy (CTE) is a progressive neurodegenerative disease believed to be the result of multiple mild traumatic brain injuries (mTBIs).
CTE was first described by Martland in 1928 as being “punch drunk,” a syndrome of confusion and ataxia in boxers having suffering repeated blows to the head.1 In 1937, Millspaugh described “dementia pugilistica,” symptoms of cognitive and motor dysfunction, once again mainly observed in boxers.
The term “chronic traumatic encephalopathy” was first coined by Miller in 1966 to encompass the mood, cognitive, and motor dysfunctions of dementia pugilistica.3 In 1973, Corsellis introduced a pattern separating CTE from other neurodegenerative diseases.
The modern definition of CTE was brought to the national spotlight by the case studies of Omalu et al. that highlighted neuropsychiatric and neuropathologic changes in National Football League (NFL) players,5 inspiring the movie “Concussion.” This article focuses on CTE in American football and why it is of importance to psychiatrists and mental health professionals.
Epidemiology and Risk Factors
The most common risk factor across case studies of CTE is a history of at least one mTBI. Onset generally occurs in mid-life, usually after retirement from professional play.6 Timing is variable, given the heterogeneity of career length among NFL players; many begin their careers in junior high school, but some start at the tender age of 6.
Of 1.2 million interscholastic football players in any given year, up to 5.6% sustain an mTBI. The majority (53%) of cases, however, remain unreported to medical personnel.
Although the literature supports a correlation between repeated mTBIs and CTE, definitive causation has not been determined.9 Still, 63% to 71% of players with repetitive mTBIs eventually develop CTE.
Among NFL players, the reported prevalence of CTE ranges from 3.7%6 to 90%.10 This disparity is largely due to disagreement among clinicians regarding what constitutes an mTBI, and the consequences faced by NFL players, their coaches, equipment managers, and team clinicians reporting them.
Players who are running-backs, begin play before age 12, and have a history of previous mTBI are at a high risk of re-injury.12 A relationship between number of years played, development of CTE, and the stage of phosphorylated Tau (pTau) pathology has also been suggested.
Retired NFL players who have had 3 or more mTBIs have a 5-fold increased risk for mild cognitive impairment, and 3-fold higher risk for depression. The APOE ε4 genotype increases the risk for cognitive impairment in CTE.
Pathophysiologic Features
Evidence suggests that repetitive disturbance of axons along with altered neurotransmission is linked to widespread glutamate release, ionic fluxes, and metabolic uncoupling.15 These changes may generate a chain of events leading to CTE.
Animal models have shown decreased serum and cerebrospinal fluid (CSF) levels and activity of tissue-nonspecific alkaline phosphatase (TNAP), an enzyme that dephosphorylates the p-Tau protein essential for microtubule assembly. Accumulation of p-Tau eventually causes neuronal death.
A recent consensus conference defined the irregular pattern of p-Tau immunoreactivity deposition surrounding microvasculature in the depths of cortical sulci as pathognomonic for CTE, a distinction from other tauopathies.
Supportive features include abnormal p-Tau neurofibrillary tangles (NFTs) distributed in layers I-II of the cortex; p-Tau thorn-like astrocytes in the subpial and periventricular regions of the cortex; pretangles, extracellular tangles, or NFTs; and dendritic swellings in the hippocampus.
Also supportive of CTE are dot-like structures and TDP-43 immunoreactive neuronal inclusions in the antromedial temporal cortex, amygdala, and the hippocampus, as well as septal abnormalities, atrophy of mammillary bodies, and third ventricle dilation.17 Staging for CTE pathology has been proposed.
There are some similarities between Alzheimer’s disease (AD) and CTE, suggesting a separate classification of CTE-AD; the presence of Aβ plaques correlates with more severe p-Tau pathology and advanced stages and clinical presentations.
Plaques in CTE-AD are more likely to be found within the sulci, contrasting with the gyral depositions observed in AD. Death tends to occur 10 years earlier, suggesting that repetitive mTBI may accelerate and change the deposition and accumulation of Aβ; presence of Aβ plaques may correlate with CTE progression and may speed up the aging process of the brain. The presence of Aβ plaques is believed to increase the odds of developing cognitive dysfunction in CTE by 4.5 times in individuals with Aβ pathology.
Although CTE cannot currently be diagnosed via imaging, there are a few PET ligands for p-Tau that show some promise. DPA-713 has detected TBI-related neuronal inflammation in 9 former NFL players with clinically-suspected CTE. The PiB amyloid ligand is also being investigated for utility in PET neuroimaging.
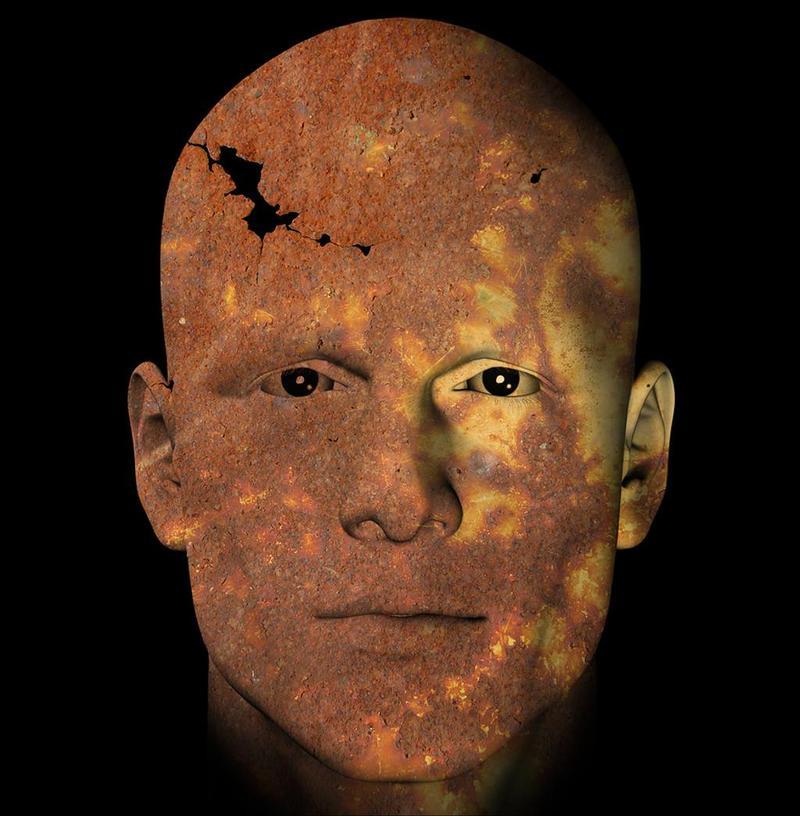
Image 1 depicts the different stages of CTE.
Neuropsychiatric Symptoms
The average age of symptom onset is between 30 and 64 years of age. Within the first 48 hours to 2 weeks after an mTBI, cognitive deficits are common.20 Four stages of neuropsychiatric symptoms were proposed in 201310, and are similar to the posthumous progression described in 2011 by Omalu et al.5
Stage I symptoms include memory loss, executive dysfunction, difficulty concentrating, inattention, aggression, depression, explosivity, and suicidality. Headache is fairly common. At this stage, very few individuals will see a psychiatrist.
by Psychiatry Advisor
Be the first to post a message!